Large bowel resection
Ascending colectomy; Descending colectomy; Transverse colectomy; Right hemicolectomy; Left hemicolectomy; Low anterior resection; Sigmoid colectomy; Subtotal colectomy; Proctocolectomy; Colon resection; Laparoscopic colectomy; Colectomy - partial; Abdominal perineal resectionLarge bowel resection is surgery to remove all or part of your large bowel. This surgery is also called colectomy. The large bowel is also called the large intestine or colon.
- Removal of the entire colon and the rectum is called a proctocolectomy.
- Removal of all of the colon but not the rectum is called subtotal colectomy.
- Removal of part of the colon but not the rectum is called a partial colectomy.
The large bowel connects the small intestine to the anus. Normally, stool passes through the large bowel before leaving the body through the anus.
Description
You'll receive general anesthesia at the time of your surgery. This will keep you asleep and pain-free.
The surgery can be performed laparoscopically, with open surgery, or robotically. Depending on which surgery you have, the surgeon will make one or more cuts (incisions) in your belly.
If you have laparoscopic or robotic surgery:
- The surgeon makes 3 to 5 small cuts (incisions) in your belly. A medical device called a laparoscope is inserted through one of the cuts. The scope is a thin, lighted tube with a camera on the end. It lets the surgeon see inside your belly. Other medical instruments are inserted through the other cuts.
- A cut of about 2 to 3 inches (in) or 5 to 7.6 centimeters (cm) may also be made if your surgeon needs to put their hand inside your belly to feel or remove the diseased bowel.
- Your belly is filled with a harmless gas to expand it. This makes the area easier for the surgeon to see and work in.
- Your surgeon examines the organs in your belly to see if there are any problems.
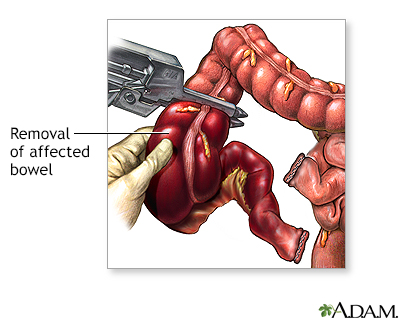
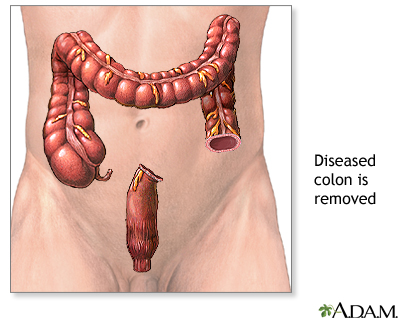
- The diseased part of your large bowel is located and removed. Some lymph nodes may also be removed.
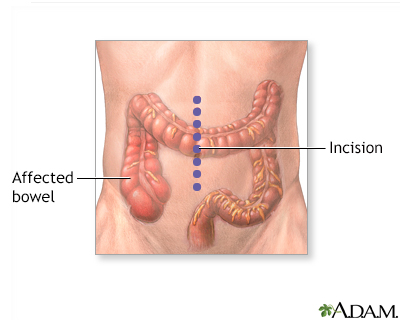
If you have open surgery:
- Your surgeon makes a cut of 6 to 8 in (15.2 to 20.3 cm) in your lower belly.
- The organs in your belly are examined to see if there are any problems.
- The diseased part of your large bowel is located and removed. Some lymph nodes may also be removed.
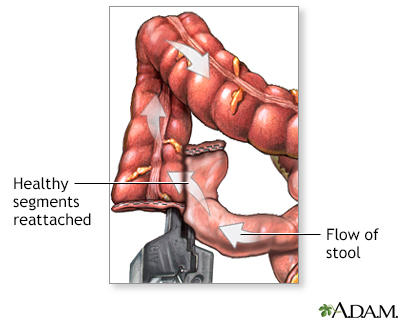
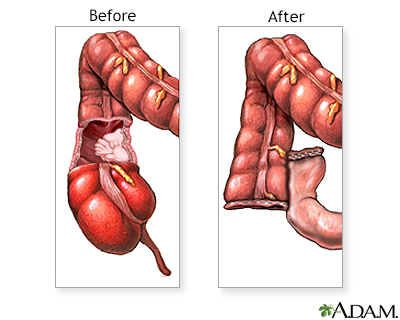
In both kinds of surgery, the next steps are:
- If there is enough healthy large intestine left, the ends are stitched or stapled together. This is called an anastomosis. Most people have this step done.
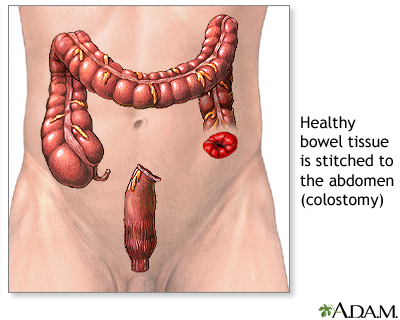
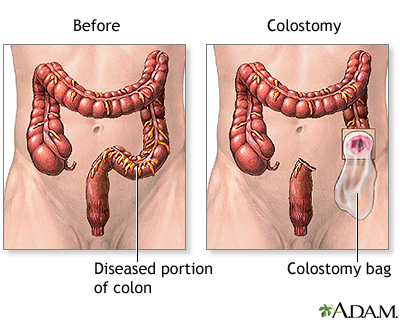
- If there is not enough healthy large intestine to reconnect, the surgeon makes an opening called a stoma through the skin of your belly. The colon is attached to the outer wall of your belly. Stool will go through the stoma into a drainage bag outside your body. This is called a colostomy. The colostomy may be either short-term or permanent. If the colostomy is short term, another surgical procedure will be needed later to reconnect the bowel and close the colostomy site.
Colectomy usually takes between 1 and 4 hours.
Why the Procedure Is Performed
Large bowel resection is used to treat many conditions, including:
- A blockage in the intestine due to scar tissue
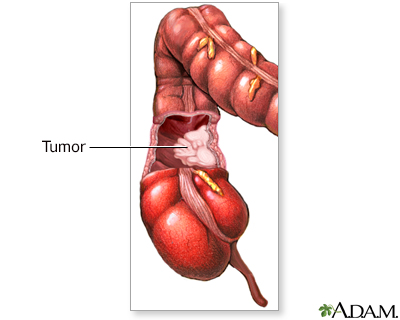
- Colon cancer
- Diverticular disease (disease of the large bowel)
Other reasons for bowel resection are:
- Familial polyposis (polyps are growths on the lining of the colon or rectum)
- Injuries that damage the large bowel
- Intussusception (when one part of the intestine pushes into another)
- Precancerous polyps
- Twisting of the bowel (volvulus)
- Ulcerative colitis
- Severe bleeding from the large intestine
- Lack of nerve function to the large intestine
Risks
Risks for anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Infection, including the lungs or bladder
- Nausea and vomiting
Risks for this surgery are:
- Bleeding inside your belly
- Bulging tissue through the surgical cut, called an incisional hernia
- Damage to nearby organs in the body
- Damage to the ureter or bladder
- Problems with the colostomy
- Scar tissue that forms in the belly and causes a blockage of the intestines
- The edges of your intestines that are sewn together come open (anastomotic leak, which may be life threatening)
- Wound breaking open
- Wound infection
-
Peritonitis
Before the Procedure
Talk with your surgeon or nurse about how surgery will affect:
- Intimacy and sexuality
- Pregnancy
- Sports
- Work
Tell your surgeon or nurse if:
- You are or could be pregnant.
- You are taking any medicines, including medicines, drugs, supplements, or herbs you bought without a prescription.
- You have been drinking a lot of alcohol, more than 1 or 2 drinks a day.
Planning for your surgery:
- If you have diabetes, heart disease, or other medical conditions, your surgeon may ask you to see the health care provider who treats you for these conditions.
- If you smoke, it's important to cut back or quit. Smoking can slow healing and increase the risk for blood clots. Ask your provider for help quitting smoking.
- If needed, prepare your home to make it easier to recover after surgery.
- Ask your surgeon if you need to arrange to have someone drive you home after your surgery.
- You may be asked to go through a bowel preparation to clean your intestines of all stool. This may involve staying on a liquid diet for a few days and using laxatives.
During the weeks before your surgery:
- You may be asked to temporarily stop taking medicines that keep your blood from clotting. These medicines are called blood thinners. This includes over-the-counter medicines and supplements such as aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and vitamin E. Many prescription medicines are also blood thinners.
- Ask your surgeon which medicines you should still take on the day of surgery.
- Let your surgeon know about any illness you may have before your surgery. This includes COVID-19, cold, flu, fever, herpes breakout, or other illness. If you do get sick, your surgery may need to be postponed.
- You may be asked to drink only clear liquids such as broth, clear juice, and water on the day before surgery.
After the Procedure
You will be in the hospital for 3 to 7 days. You may have to stay longer if the colectomy was an emergency operation.
You may also need to stay longer if a large amount of your large intestine was removed or if you develop problems after the surgery.
By the second or third day, you will probably be able to drink clear liquids. Thicker fluids and then soft foods will be added as your bowel begins to work again.
After you go home, follow instructions on how to take care of yourself as you heal.
Outlook (Prognosis)
Most people who have a large bowel resection recover fully. Even with a colostomy, most people are able to do the activities they were doing before their surgery. This includes most sports, travel, gardening, hiking, other outdoor activities, and most types of work.
If you have a long-term (chronic) condition, such as cancer, Crohn disease, or ulcerative colitis, you may need ongoing medical treatment.
References
Albers BJ, Lamon DJ. Colon repair/colostomy creation. In: Baggish MS, Karram MM, eds. Atlas of Pelvic Anatomy and Gynecologic Surgery. 5th ed. Philadelphia, PA: Elsevier; 2021:chap 96.
Galandiuk S, Netz U, Morpurgo E, Tosato SM, Abu-Freha N, Ellis CT. Colon and rectum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. Philadelphia, PA: Elsevier; 2022:chap 52.

















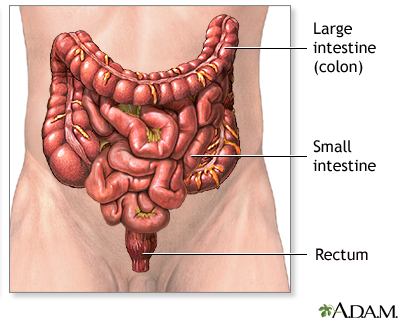
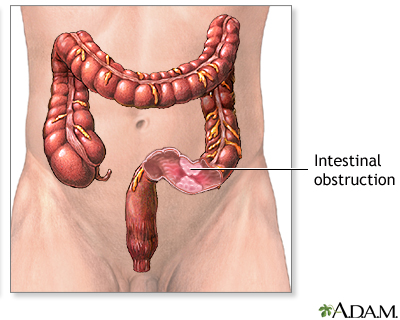

![<strong>Large bowel resection - series</strong><p>The large bowel [large intestine or the colon] is part of the digestive system. It runs from the small intestine to the rectum. It is made up of three portions; the ascending, transverse and descending colon. The ascending colon is sometimes referred to as the right colon; the descending colon is sometimes referred to as the left, or sigmoid colon.</p>](../../graphics/images/en/10255.jpg)